Welcome "Rheumatoid Arthritis" sufferers
It’s past time to stop the pain!
I'm Laura Thornton co-founder of the
Pain Cure Clinic in Boulder, Colorado and
I struggled with (what I thought was!) RA
for three. long, frustrating decades.
Congratulations for finding your way to this mind-body approach to healing and to our site!
Now, you may have some questions - I certainly did when first hearing about
Dr. Sarno and Tension Myositis Syndrome (TMS).
So let's answer some of the most frequently asked questions about RA and TMS.
FAQ #1: Unlike the structural changes that Dr. Sarno talks about (that aren’t, in fact, causing chronic pain), isn’t RA an actual disease process? My doctor says RA can be genetic and there’s no cure. My mother has it too.
All good points. But isn’t it also entirely plausible that this “disease” is actually, literally exactly what it sounds like: DIS-EASE? A lack of satisfaction and fluidity with some things in your life that are causing you stress and keeping your muscles contracted.
And what else do you have in common with your mother – a tendency to be your own worst critic perhaps? A habit of taking on too much, for too long – the inability to say “no”? You may very well have inherited a condition from your lovely mama, but it’s TMS not RA!
FAQ #2: How can emotional stress cause pain and inflammation in my body?
In a nutshell: over time, our ancestors developed a defense system (by way of the autonomic nervous system) that would spring the body into action whenever there was a physical threat. Physiological responses to danger, like muscle contraction, would prepare the body to fight or flee.
The problem in modern society is that much of the stress that we experience on a day-to-day basis is no longer acute (as in short-term and quickly resolved). We live in a time when stressors are coming at us all day long. And when stress becomes chronic (as it does with all TMS sufferers), then your muscle and other soft tissue tightness and inflammation also become chronic - and this leads to ongoing pain that gets labeled as RA or another chronic condition.
To wrap up this answer: here’s an example of acute stress vs. chronic stress. A disagreement with your sister (with whom you usually have a good relationship) over where to go to celebrate your parent’s 50th wedding anniversary is a temporary issue, likely quickly resolved; therefore, acute stress. While your mother-in-law continually questioning and correcting your parenting skills is a slow drip of chronic stress. See the difference? Dealing with acute stress is built into our DNA, but longer-term tension will eventually send you a warning flare in the form of a chronic physical condition.
FAQ #3: Ok but. in addition to pain. I have swelling, fluid around some of my joints or even real joint damage!
I hear you. The onset of my pain involved a swollen, painful, fluid filled knee. Very uncomfortable and scary. Tense, inflamed soft tissue can swell and collect fluid. Think about what happens with a real injury, such as a twisted ankle. An injury creates a similar physiological response, that’s acute vs. TMS, which builds over time.
Let’s take a look at the anatomy of a knee for example:
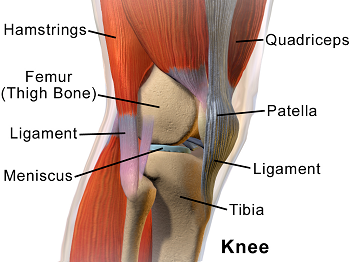
The knee is a large, complicated joint and the soft tissue surrounding your knee plays an important supporting role. This graphic doesn’t show everything, but we’ve got muscles, tendons, ligaments, and nerves in play here. When I had chronic pain, I remember thinking, it seems like the discomfort is coming from the area around my joint – an interesting observation, knowing what I know now about TMS. I also had pain in my upper chest area, where there are no moving parts, but plenty of soft tissue, and that just never made sense to me with an RA diagnosis.
And finally, let me address joint damage by first saying that my heart aches for any of you who are living with this situation. Unfortunately, prolonged inflammation can cause actual structural changes. I’m grateful to just have a little lasting damage myself. While we can’t undo existing damage, getting rid of inflammation can keep it from getting worse. And give you what you deserve – a chronic pain free life moving forward.
FAQ #4: How come some medications work to reduce my pain?
Listen, almost everyone diagnosed with RA initially turns to medication to ease the pain and to function. As you likely know, there are two primary categories of medication for arthritis: anti-inflammatories, formally called non-steroidal anti-inflammatory drugs and biologics, often administered by injection which, they claim slowS the progression of the “disease.” There are others drugs, such as cortisone – taken orally as Prednisone or given as a shot for quick, albeit temporary relief. And even Methotrexate – a cancer drug. I was on all of these medications (and more!) at one time or another during my three decades living with RA.
So the thing is, Drugs can and do work to reduce your symptoms to a certain extent. Though the effectiveness can be hit or miss and many of us pay the price with nasty side effects. In addition, there’s the Placebo Effect, which I expect most of you are, at least somewhat, familiar with. You’re told a drug will work, you desperately want it to work, so it does – at least for a while.
Here’s how that looked for me. I would have a flare up – sometimes after being in remission for years. I’d go back on one of the disease modifying drugs that they say takes 4-6 weeks to reach full effectiveness and I would literally keep track of each week on paper, counting the days until the drug would start working. Hmmm – what do you think happened? At just about the 4-week mark, my pain would start reducing. But do you know what else happened during that time? My stress level decreased because I now had the “magic pill” – also, I often had dealt with the stressor in my life that had ignited my flare up in the first place. So, I now wonder, what was really working to resolve my pain?
Now I’m not a doctor, so I can’t advise you, specifically, about how or when to wean off your medication, but I can tell you that you can start this mind-body process of healing while still taking your medication. The idea is not to be a martyr or suffer unnecessarily. Just start thinking of your current medical treatment as temporary and no longer a life sentence.
FAQ #5: I’ve gone into remission before. Why can’t I get over RA with just “willpower”?
I can so relate - I had willpower in spades! But willpower alone was never enough to keep my chronic pain from returning – sometimes years later, but it always came back on the heels of a significant stressor in my life. Here’s the thing: you’ve got to look at the big picture - all areas of your life - to permanently banish chronic pain. For instance: Perfectionist Personality anyone?
This process is not overly complicated but, I won’t lie, it means going against the herd. But, make no mistake, the RA herd you’re hanging out with right now is headed right toward the cliff. The way out of this is to veer off from the herd and commit to a mind-body approach. The bottom line is that I’m likely very much like you. I don’t have some special power that made it possible for me to cure RA that you don’t have. We ALL have the potential to take an alternate mind-body path and heal.
And by the way, I have the real definition for remission - it’s simply physical, mental and life circumstance related stress reduction!
Coaching services offered by the Pain Cure Clinic are not intended as medical advice or professional psychotherapy. This is practical knowledge based on experience about how to alternately eliminate chronic pain symptoms caused by psychological factors. Medical or mental health questions or diagnosis should be directed to your physician or psychologist. The Pain Cure Clinic is not endorsed by or affiliated with Dr. John Sarno. Individual results will vary.

